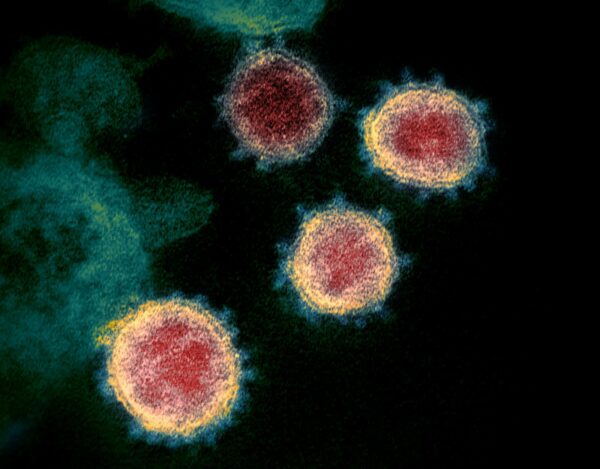
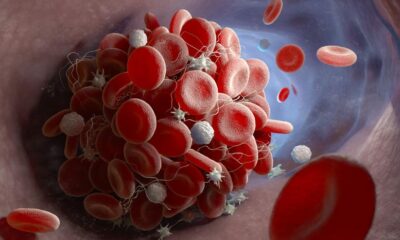
The review, which was peer looked into and uncovered in the diary “Nature Communications,” began in September 2020 and looked at 52 family contacts of individuals that had inspected hopeful for COVID-19. It found that 26 people who have been uncovered to the Covid anyway didn’t become ill had significantly bigger cross-receptive T-cells, produced by prior normal colds, than those that transformed into in chronic frailty with COVID.
Lymphocytes created as a feature of the body’s normal insusceptible reaction to the normal virus might help shield against difficult disease from COVID-19, as indicated by a review did in the U.K. Analysts at Imperial College London told News the discoveries could assist researchers with making antibodies that stay more compelling against new variations of the Covid.
This is so for various reasons, including that not all colds are brought about by Covids, and T-cells’ capacity to ward off suggestive contaminations disappears after some time.
“The end ought not be that assuming you’ve had a typical cold you don’t have to stress over contracting COVID-19,” Professor Aljit Lalvani, one of the creators of the review, told News.
Lalvani said most of the current COVID-19 antibodies explicitly focus on the infection’s spike protein, which it uses to append itself to sound human cells. The immunizations make the body produce antibodies and T-cells that react to that protein. This has offered great security against the Covid up until this point, however as has been seen with Omicron, different changes to the spike protein can deliver the antibodies less compelling.
“The way that (the T-cells) can assault the interior proteins of each of these related infections [COVID-19 variants] implies that they give what’s known as an expansive cross-insurance,” Lalvani told News. “That is in sharp differentiation to the surface spike protein, which is the objective of antibodies instigated by immunizations. What’s more plainly, SARS-CoV-2 is under tremendous, serious tension in the worldwide populace on the grounds that a great many people currently have these antibodies, regardless of whether actuated by immunization or contamination, so the infection is attempting normally to dodge that invulnerability through transformation, and that is the reason Omicron has such countless changes in the spike protein. Yet, the inner proteins are generally unaltered.”
“Everything the review says to us is that there is a component, a characteristic instrument of regular defensive insusceptibility, that is set off by past normal cold Covid diseases. … So the point isn’t to depend on that, however to take advantage of and to outfit that normally happening defensive resistance to foster better antibodies.”
Lalvani says the examination at Imperial College found that T-cells created after a typical virus brought about by other Covids (which are normal) assault a sort of proteins that stay comparative across the known COVID-19 variations. These inner proteins are answerable for infection replication, rather than appending to outer cells. That indispensable job in the infection’s advancement gives it undeniably less potential to transform, he clarified.
“This is presently a conclusive green light to push ahead and foster a T-cell inciting immunization to interior center proteins, which ought to secure against current and future variations,” he said. “We’re extremely lucky to have observed what immunologists allude to as the ‘Sacred goal,’ so we’re sharp for individuals to get this and to see that, finally, there is a way towards managing future variations.”
Lalvani said the review should influence how researchers approach the improvement of future COVID immunizations.

 Health4 weeks ago
Health4 weeks ago
 Technology4 weeks ago
Technology4 weeks ago
 Sports4 weeks ago
Sports4 weeks ago
 Science4 weeks ago
Science4 weeks ago
 Business2 weeks ago
Business2 weeks ago
 Science2 weeks ago
Science2 weeks ago
 Science2 weeks ago
Science2 weeks ago
 Technology2 weeks ago
Technology2 weeks ago