Health
New exploration points to vagus nerve harm as justification for long COVID
Published
3 years agoon
The review recommended that SARS-CoV-2 intervened vagus nerve brokenness (VND) could be answerable for long COVID.
New exploration to be introduced at the current year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID 2022, Lisbon, 23-26 April) proposes that large numbers of the manifestations associated with post-COVID condition (PCC, otherwise called long COVID) could be connected with the impact of the infection on the vagus nerve – one of the most significant multi-useful nerves in the body. The review is by Dr Gemma Lladós and Dr Lourdes Mateu, University Hospital Germans Trias I Pujol, Badalona, Spain, and associates.
Numerous indications of Post-COVID-19 condition could be brought about by enduring harm supported to one of the main nerves in the human body during introductory contamination with Covid, new examination has recommended.
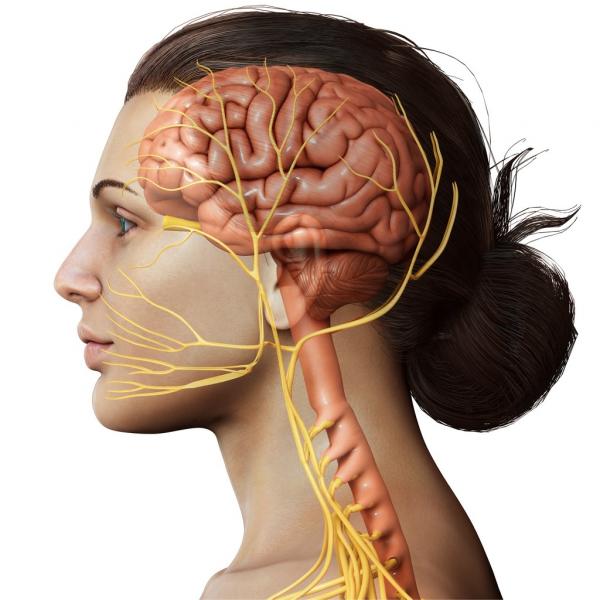
The vagus nerve reaches out starting from the brain into the middle and into the heart, lungs and digestive organs, as well as a few muscles incorporating those associated with gulping. All things considered, this nerve is liable for a wide assortment of normalphysical processes including controlling pulse, discourse, the gag reflex, moving food from the mouth to the stomach, moving food through the digestive organs, perspiring, and numerous others.
The vagus nerve is the tenth cranial nerve and is the longest and generally complex of every one of them. It runs from the mind all through the sum of the face and chest, arriving at the mid-region. The vagus nerve fills in as the fundamental association between the mind and the gastrointestinal lot, sending back data about the condition of the inward organs.
Long COVID is a possibly impairing disorder influencing an expected 10-15% of subjects who endure COVID-19. The creators suggest that SARS-CoV-2-interceded vagus nerve brokenness (VND) could clarify some lengthy COVID indications, including dysphonia (industrious voice issues), dysphagia (trouble in gulping), tipsiness, tachycardia (unusually high pulse), orthostatic hypotension (low circulatory strain) and looseness of the bowels.
As well as being essential to the gastrointestinal framework as it controls the exchange of food from the mouth to the stomach and moves food through the digestive organs, the vagus nerve is likewise liable for a long time cycles, for example, controlling the pulse, sweat creation and the gag reflex, as well as specific muscle developments in the mouth, including those fundamental for discourse.
The creators played out a pilot, broad morphological and useful assessment of the vagus nerve, involving imaging and useful tests in an imminent observational accomplice of long COVID subjects with indications reminiscent of VND. In their complete companion of 348 patients, 228 (66%) had somewhere around one side effect reminiscent of VND. The current assessment was acted in the initial 22 subjects with VND manifestations (10% of the aggregate) found in the Long COVID Clinic of University Hospital Germans Trias I Pujol among March and June 2021. The review is progressing, and keeps on enrolling patients.
New examination set to be introduced at the current year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) researches the association between Post-COVID-19 disorder, otherwise called long COVID, and the vagus nerve.
Of the 22 subjects dissected, 20 (91%) were ladies with a middle age of 44 years. The most successive VND-related manifestations were: the runs (73%), tachycardia (59%), tipsiness, dysphagia and dysphonia (45% each), and orthostatic hypotension (14%). Practically every one of the (19 subjects, 86%) had something like 3 VND-related side effects. The middle earlier term of indications was 14 months. Six of 22 patients (27%) showed adjustment of the vagus nerve in the neck shown by ultrasound – including both thickening of the nerve and expanded ‘echogenicity’ which demonstrates gentle provocative receptive changes.
A thoracic ultrasound showed straightened ‘diaphragmatic bends’ in 10 out of 22 (46%) subjects (which deciphers an abatement in diaphragmatic versatility during breathing, or all the more just unusual relaxing). A sum of 10 of 16 (63%) evaluated people showed decreased most extreme motivation pressures, showing shortcoming of breathing muscles.
The review proposes that SARS-CoV-2-interceded vagus nerve brokenness (VND) could be liable for a significant number of the indications of long COVID, including industrious voice issues, trouble gulping, wooziness, strangely high pulse (tachycardia), low circulatory strain and stomach related issues.
Eating and stomach related capacity was additionally impacted in certain patients, with 13 of 18 evaluated (72%) having a positive screen for self-saw oropharyngeal dysphagia (inconvenience gulping). An evaluation of gastric and inside work acted in 19 patients uncovered 8 (42%) had their capacity to convey food to the stomach (by means of the throat) debilitated, with 2 of these 8 (25%) announcing trouble in gulping. Gastroesophageal reflux (heartburn) was seen in 9 of 19 (47%) people; with 4 of these 9 (44%) again experiencing issues conveying food to the stomach and 3 of these 9 (33%) with hiatal hernia – which happens when the upper piece of the stomach swells through the stomach into the chest hole.
Long COVID is a condition described by persevering and persistent medical problems brought about by COVID-19 after the patient has recuperated from the underlying diseases. It can influence practically every organ in the body, as well as cause a scope of psychological wellness and sensory system issues. The absolute most normal manifestations of long COVID incorporate weariness, migraines, windedness, loss of smell and taste, and muscle shortcoming.
To additionally comprehend the peculiarity, the specialists utilized imaging and practical tests, as well as a morphological and utilitarian assessment of the vagus nerve, in an evaluation of long COVID patients introducing at least one indications of VND.
A Voice Handicap Index 30 test (a standard method for estimating voice work) was unusual in 8/17 (47%) cases, with 7 of these 8 cases (88%) enduring dysphonia.
Numerous patients likewise showed changes in stomach related capacity, with 13 of 18 surveyed (72%) additionally having a positive evaluating for oropharyngeal dysphagia, or inconvenience gulping, which can influence the stomach related cycle. Eight patients gave indications of decreased or disabled capacity to convey food to the stomach by means of the throat, with others experiencing indigestion.
You may like
-


Coronavirus in India LIVE updates: India reports 13,313 new cases and 38 deaths in last 24 hours
-

Covid cases rising again: India Records 12,847 New Covid Cases In 24 Hours is it a wave?
-


Most unvaccinated kids absence antibodies after COVID
-

The top omicron and delta variation side effects to know as deltacron arises
-

The most up-to-date COVID variation was lurked for almost a year
-


as per research , coronavirus is connected to long haul psychological wellness issues in recuperated patients
Health
Fruits High in Protein: A Surprising Nutritional Boost
Published
4 months agoon
January 20, 2025
When thinking of protein sources, fruits might not top the list. However, certain fruits can contribute a surprising amount of this essential macronutrient. While they can’t replace traditional high-protein foods like beans, legumes, or meats, these fruits provide a valuable combination of protein, fiber, vitamins, and antioxidants. Here’s a closer look at protein-rich fruits and their nutritional benefits.
Why is Protein Important?
Protein plays a crucial role in maintaining satiety, tissue repair, and muscle growth. High-protein diets are widely known for aiding weight loss and supporting a healthy lifestyle. Recently, plant-based diets have gained attention for their weight loss benefits and overall health advantages.
Registered dietitian Natalie Rizzo emphasizes that fruit protein should be seen as an addition rather than a primary source. “Every gram of protein counts, especially in a plant-forward diet,” she says. Most people need at least 20 grams of protein per meal, and fruits can be a small yet beneficial contributor.
Protein-Rich Fruits
Here are some fruits that stand out for their protein content, with each providing 1 gram or more per serving.
Passion Fruit
- Protein: 5 grams per cup of raw fruit
- Known for its aromatic, jelly-like golden pulp, passion fruit is also rich in fiber, calcium, and vitamins A and C. It can be eaten raw, added to yogurt, or blended into drinks.
Jackfruit
- Protein: 2.8 grams per cup of raw slices
- A relative of figs and breadfruit, jackfruit can be eaten ripe as a sweet fruit or unripe as a meat alternative in plant-based dishes.
Pomegranate
- Protein: 2.9 grams per cup of arils (seeds)
- Pomegranate seeds are packed with antioxidants, dietary fiber, and anti-inflammatory fatty acids beneficial for heart health.
Apricots
- Protein: 2.3 grams per cup of fresh slices; 4.4 grams per cup of dried halves
- This fiber-rich stone fruit also provides antioxidants, iron, and vitamins C, E, B6, and A. Fresh or dried, apricots are a delicious and nutritious snack.
Blackberries
- Protein: 2 grams per cup of raw fruit
- Blackberries are rich in antioxidants that may reduce cancer risk and improve gut health due to their high fiber content.
Guava
- Protein: 1.4 grams per fruit
- This tropical fruit offers antioxidants, vitamin C, potassium, and fiber. Its sweet-tart flavor makes it versatile for eating raw, blending into smoothies, or making jams.
Raisins
- Protein: 1.4 grams per 1.5-ounce box
- Raisins are small but mighty, offering fiber, potassium, and heart health benefits. They make a convenient and nutrient-dense snack, but portion control is key due to their calorie content.
Citrus Fruits
- Protein: 1.2 grams per orange; 2.3 grams per grapefruit
- Famous for their vitamin C content, oranges and grapefruits also deliver fiber, potassium, and hydration while being low in calories.
Cantaloupe
- Protein: 1.3 grams per cup of cubed fruit
- A standout for its high vitamin A content, cantaloupe provides 40% of the daily recommended intake per cup. It’s an excellent addition to fruit salads, smoothies, or desserts.
Incorporating Fruits Into a Protein-Rich Diet
While fruits shouldn’t be relied on as a primary protein source, they can complement a balanced diet rich in beans, nuts, seeds, and other plant-based proteins. Their added benefits—like vitamins, antioxidants, and fiber—make them a healthy, versatile choice.
Whether you’re blending blackberries into a smoothie, topping yogurt with passion fruit pulp, or snacking on a handful of raisins, these protein-rich fruits are a simple way to enhance your diet while satisfying your sweet tooth.
Health
Coffee and Tea Drinking May Reduce the Risk of Some Cancers: Research
Published
5 months agoon
December 25, 2024
Drinking a cup of Joe or some tea for the holidays may be a good thing!
A study reviewed in the journal of the American Cancer Society found that people who drink either tea or coffee have a slightly lower risk of head and neck cancers, though it remains unclear if the drinks themselves directly reduce the risk.
Researchers analyzed data from 14 individual studies involving over 9,500 people with head and neck cancers and over 15,000 people without, compiled by the International Head and Neck Cancer Epidemiology Consortium.
The findings showed that individuals who drank less than four cups of caffeinated coffee daily and less than a cup of tea had a 17% and 9% lower chance, respectively, of developing head or neck cancer overall.
The study also highlighted that coffee drinkers had a reduced risk of developing oral cavity and oropharyngeal cancers located in the middle part of the throat, according to Yale Medicine. Meanwhile, tea drinkers who consumed less than a cup daily showed a lower risk of hypopharyngeal cancer, which affects the bottom part of the throat, per Johns Hopkins Medicine.
“While there has been prior research on coffee and tea consumption and reduced risk of cancer, this study highlighted their varying effects with different sub-sites of head and neck cancer, including the observation that even decaffeinated coffee had some positive impact,” said Dr. Yuan-Chin Amy Lee, senior author of the study from Huntsman Cancer Institute and the University of Utah School of Medicine, as reported by The Guardian.
“Perhaps bioactive compounds other than caffeine contribute to the potential anti-cancer effect of coffee and tea,” Lee added.
However, drinking more than one cup of tea daily was linked to a higher risk of laryngeal cancer, which forms in the larynx, the part of the throat responsible for controlling the vocal cords, according to the National Cancer Institute (NCI).
The study also acknowledged limitations, as participants self-reported their findings and were not asked about the specific types of tea or coffee consumed. Additional unaccounted factors may have influenced the results as well.
“In observational studies, it is very difficult to totally eliminate confounding effects, for example, of tobacco and alcohol from the statistical analysis,” Tom Sanders, a professor emeritus of nutrition and dietetics at King’s College London, told The Guardian.
“Consequently, people who drink a lot of coffee and tea may be more likely to avoid other harmful behaviors such as drinking alcohol and using tobacco and so may be at a lower risk of these cancers for other reasons,” added Sanders, who was not involved in the study.
Health
How the brain makes complex judgments based on context
Published
5 months agoon
December 16, 2024
We frequently face difficult choices in life that are impacted by a number of variables. The orbitofrontal cortex (OFC) and the dorsal hippocampus (DH) are two key brain regions that are essential for our capacity to adjust and make sense of these unclear situations.
According to research conducted by researchers at the University of California Santa Barbara (UCSB), these regions work together to resolve ambiguity and facilitate quick learning.
Decision-making that depends on context
The results, which were released in the journal Current Biology, offer fresh perspectives on how certain brain regions assist us in navigating situations that depend on context and modifying our behavior accordingly.
According to UCSB neuroscientist Ron Keiflin, senior author, “I would argue that that’s the foundation of cognition.” That’s what prevents us from acting like mindless machines that react to stimuli in the same way every time.
“Our ability to understand that the meaning of certain stimuli is context-dependent is what gives us flexibility; it is what allows us to act in a situation-appropriate manner.”
Decision-making context
Think about choosing whether or not to answer a ringing phone. What you say depends on a number of variables, including the time of day, who might be calling, and where you are.
The “context,” which influences your choice, is made up of several components. The interaction between the OFC and DH is what gives rise to this cognitive flexibility, according to Keiflin.
Planning, reward valuation, and decision-making are linked to the OFC, which is situated directly above the eyes, whereas memory and spatial navigation depend on the DH, which is positioned deeper in the brain.
According to Keiflin, both areas contribute to a mental representation of the causal structure of the environment, or a “cognitive map.” The brain can model outcomes, forecast outcomes, and direct behavior thanks to this map.
Despite their significance, up until now there had been no systematic testing of the precise functions of these regions in contextual disambiguation, which determines how stimuli alter meaning based on context.
Contextualizing auditory stimuli
In order to find out, the researchers created an experiment in which rats were exposed to aural cues in two distinct settings: a room with bright lighting and a chamber with no light. There was a context-dependent meaning for every sound.
For instance, one sound indicated a reward (sugar water) only when it was light, and another only when it was dark.
The rats eventually learnt to link each sound to the appropriate context, and in one situation they showed that they understood by licking the reward cup in anticipation of a treat, but not in the other.
The OFC or DH was then momentarily disabled during the task by the researchers using chemogenetics. The rats’ ability to use context to predict rewards and control their behavior was lost when the OFC was turned off.
Disabling the DH, however, had minimal effect on performance, which was unexpected considering its well-established function in memory and spatial processing.
Enhanced learning from prior knowledge
For learning new context-dependent interactions, the DH proved essential, but it appeared to be unnecessary for recalling previously learned ones.
“If I walked into an advanced math lecture, I would understand – and learn – very little. But someone more mathematically knowledgeable would be able to understand the material, which would greatly facilitate learning,” Keiflin explained.
Additionally, the rats were able to pick up new relationships far more quickly after they had created a “cognitive map” of context-dependent interactions. The duration of training decreased from more than four months to a few days.
Brain areas cooperating
By employing the same chemogenetic strategy, the researchers discovered that the rats’ capacity to use past information to discover new associations was hampered when the OFC or DH were disabled.
While the DH allowed for the quick learning of novel context-dependent relationships, the OFC was crucial for using contextual knowledge to control immediate action.
This dual role emphasizes how these brain regions assist learning and decision-making in complementary ways.
Education and neuroscience Implications
According to Keiflin, neuroscience research frequently overlooks the well-established psychological and educational theories that prior information affects learning.
Knowing how the brain leverages past information to support learning could help develop educational plans and therapies for people who struggle with learning.
The study clarifies the different functions of the DH and OFC as well. In order to acquire new relationships, the DH is more important than the OFC, which aids in behavior regulation based on contextual knowledge.
These areas work together to help the brain adjust to complicated, dynamic surroundings.
Brain’s Capacity to make Decisions based on context
The study emphasizes how crucial contextual knowledge is for managing day-to-day existence. Human cognition is based on the brain’s capacity to resolve ambiguity, whether it be while choosing whether to answer a ringing phone or when adjusting to new knowledge.
This work highlights the complex processes that facilitate learning and decision-making while also advancing our knowledge of brain function by elucidating the functions of the OFC and DH.
This information creates opportunities to investigate the potential roles that disturbances in these systems may play in disorders like anxiety or problems with decision-making.
Since this type of learning is most likely far more reflective of the human learning experience, Keiflin stated that “a better neurobiological understanding of this rapid learning and inference of context-dependent relations is critical, as this form of learning is probably much more representative of the human learning experience.”
The results open the door for future studies on the interactions between these brain areas in challenging, real-world situations, which could have implications for mental health and education.
